|
|
Haemorrhoids or Piles |
|
Modern Understanding and Treatment of Piles or Haemorrhoids
Piles or haemorrhoids (Blood Flowing in Greek as described by Hippocrates) are one of the most common afflictions of Singaporeans. In the West, it has been estimated that at least 50% of individuals over the age of 50 years have at some time experienced piles complaints. Although we do not have the figure for Singapore, the experience here is probably similar. Piles can occur at any age and affect both sexes.
|
|
What are Piles?
Piles for many years were wrongly described as engorged or varicose veins of the anal canal. From recent detailed scientific studies, we now realise that piles are due to displaced and enlarged normal structures at the lower end of the rectum called “anal cushions”.
Anal cushions are thickenings in the internal lining of the lower part of the rectum, they contain blood vessels (both arteries and veins), elastic and fibrous tissues. These tissues anchor the anal cushions to the wall of the lower rectum and upper anal canal. Everybody including newborn babies have anal cushions. They give us the ability of very fine control of the anal sphincter, not unlike the “washer” in a tap. They become piles when they are enlarged and displaced downwards, but if completely excised, we could lose 20% of anal sphincter control. |
| |
| What are the causes of piles? |
| |
Piles are not caused by sitting on hot seats! They are caused by poor bowel habit like chronic straining at stools, constipation, sitting on the toilet for a long time (reading and listening to music!). In women, pregnancy and childbirth can cause piles or aggravate symptoms of piles. Piles often run in families, therefore hereditary may be an important factor especially in those who acquire piles at an early age. |
| |
| What are the symptoms of piles? |
| |
The commonest symptom is painless fresh bleeding when passing motion. Piles can also cause itchiness, protrusion (prolapse) which sometimes has to be pushed back, mucus discharge and discomfort. Piles are rarely painful unless complications like clotting of blood or infection occur.
These symptoms are not specific to piles : other conditions like fissure (tear), blood clot (perianal haematoma), infection and inflammation of the rectum, anus or surrounding skin fistula (opening by the side of the anus), and of course cancer of the anus or rectum can also mimic symptoms of piles. Therefore it is important to get such symptoms carefully checked by a doctor.
|
| |
| Can piles turn into Cancer? |
| |
Piles will not turn into cancer but symptoms such as bleeding when passing motion can be due to both piles or cancer. It is not uncommon for patients to assume that their bleeding is due to piles and not bother to seek medical attention until the cancer has become very advanced. |
| |
| How are piles treated? |
| |
| Not all piles are the same and they are not treated the same way. Treatment depends on the severity or Grades of piles, which are also referred to as “degrees of piles”. |
| |
| Grades of Piles |
| |
| • |
- No prolapse. Piles remain internal
|
| • |
- Prolapse when passing motion but they retract back on their own
|
| • |
- Prolapse but needs to be pushed back
|
| • |
- Prolapse but cannot be pushed back
|
|
| |
Unfortunately, no single grading system can cover all the different presentations of piles encountered in clinical practice. Most Singaporeans have problem with piles for many years by the time they see their colorectal surgeons. Such chronic piles often have other features like large and ugly skin tags, external piles, firm polyp-like lumps (called fibroepithelial polyps and hypertrophic papillae), or co-existing conditions like fissures and fistulae. The typical text book illustration of piles is a set of three following the three main blood vessels supplying the anal cushions : chronic piles can be more than three or even circumferential i.e. protrusion of a complete ring of piles like those experienced by some women immediately after giving birth.
Small Grade I piles are treated by high fibre diet and suppository only or by injection with a schlerosant agent (5% Phenol in vegetable oil). This is injected just above the piles, it causes inflammation and fibrosis resulting in shrinkage of the piles and “plastering” back the anal cushion to their normal positions.
Large Grade I, Grade II and small Grade III piles with minimal external or polyp-like components are treated by ligation or rubber banding. With ligation, the piles tissue is pulled into the “drum” of a simple device and 2 small rubber bands are then tightly applied to the base. This squeezes on the blood supply in the piles tissue. It drops off after one week leaving an ulcer, which takes another week or two to heal. The procedure shaves or trims off extra tissue of the anal cushion, subsequently healing helps to fix the remaining anal cushion into its usual position.
Both injection and ligation are performed in the clinic or doctor’s office. But they must be done only on internal piles. If external piles or skin tags, which have very sensitive nerve ends, were treated this way, it would be extremely painful and unbearable.
Large Grade III, Grade IV or piles with symptomatic external components or polypoid masses require surgery. |
| |
| Pain and Piles Surgery or Haemorrhoidectomy |
| |
Piles surgery traditionally is reported to be one of the most painful procedures. Many patients would have heard stories from friends or relatives of severe pain especially during passing motion lasting for weeks. Frequently, the “fear of pain” prevents patients from accepting surgery preferring instead to put up with the inconvenience, embarrassment and the suffering from their piles. |
| |
| Conventional Piles Surgery |
| |
Conventional piles surgery involve the cutting of piles from the sensitive anal skin outside to the interior of the anal canal. The anal skin and the lower half of the anal canal, like the lips and mouth, is a very sensitive part of the body rich in sensory nerve endings. Any cut on such surface is extremely painful especially if accompanied by inflammation and infection.
Over the years, colorectal surgeons have been trying to reduce this terrible pain. One way is by doing meticulous surgery with diathermy, “an electric knife”, and by judicious use of painkiller, anal muscle relaxant and stool softener. Other methods include Laser or ultrasonics machines like Harmonic scalpel or Ligasure. But pain remains a big problem.
To have painless piles surgery, a radical and revolutionary approach is needed. |
| |
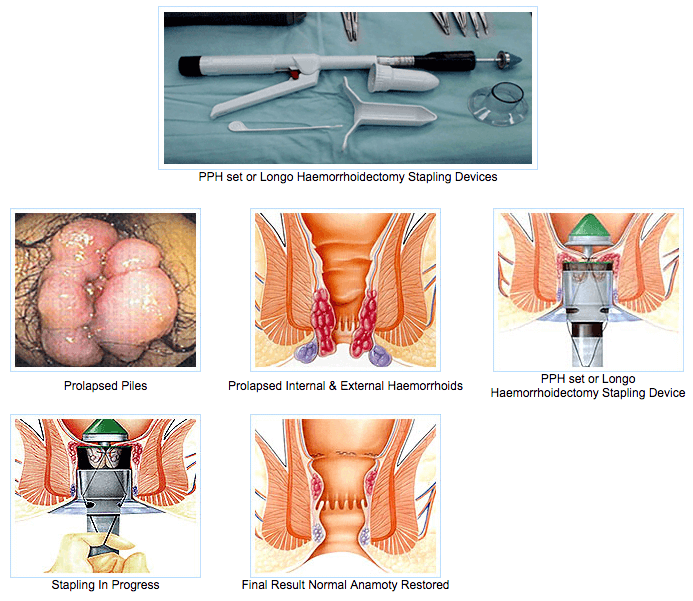
| Longo Stapled Haemorrhoidopexy– the "painless" piles surgery |
| |
Dr Longo is an Italian surgeon who introduced his technique to the world in June 1998 in Rome. He reasoned that since piles are due to prolapse or displacement of enlarged and engorged anal cushions from the junction of anus and rectum, why not pull them up to their normal positions from the inside instead of cutting them out from the outside. If at the same time, you could cut down the flow of the very rich blood supply, you would reduce the congestion and cause the piles to regress and shrink. This method aims to restore the anatomy to normal.
The Beauty of this approach is that cutting is on rectal mucosa and submucosa, tissues which carry no sensory nerve endings, so it should be relatively painfree.
Longo stapled haemorrhoidopexy uses a purpose designed staple device to cut a 2 cm circumferential sleeve of lining of the rectum to pull up the displaced piles to their normal positions, and reduce their blood supply. Over a few days or weeks, the piles will regress to normal. Because of the circumferential cut, all piles are treated, unlike conventional surgery when smaller piles are often left behind to grow giving them a chance to recur.
The bonus of this procedure is once the exteylal piles are also pulled inside reducing the external bulk. Only the large skin tags will remain. In Singapore, our patients prefer to have a relatively smooth bottom following surgery. These skin tags can be trimmed and sutured nicely as in cosmetic surgery. For most patients, this adds only a little pain to the overall procedure.
The other advantage of this procedure is that patients can be discharged the same day or one day later and return to normal activity much quicker, average 4 days to one week instead of two to three weeks for conventional surgery. |
| |
 |
| |
| Possible Complications |
| |
Like every operation, certain possible complications might occur with the Longo Stapled Haemorrhoidopexy.
Minor complications include minor bleeding, mild pulling sensation in the abdomen or in the rectum in the first few days, retention of urine especially in older male patients and mild soft stricture or narrowing of the rectum.
More serious complications include secondary haemorrhage (major bleeding occurring 5-7 days following surgery), significant fibrous stricture of the rectum and troublesome spasm of the anal canal. Most serious complications include infection inside the abdomen, injury and perforation to the rectum. Fortunately such severe complications are extremely rare.
Nevertheless, this procedure must be performed with care and attention to detail to minimise the risk of severe complications.
Longer term results (ie five year after surgery) are being reported with some claming satisfactory long term results while others showing a higher recurrence rate of piles when compared with conventional excisional surgery. This is probably due to surgical technique : large external piles and skin tags when they are just pushed up into the anal canal will just come out again with time, they need to be trimmed.
It is important to stress that treatment of piles either by injection, ligation or surgery is only one part of piles management, the other part is to ensure that patient cultivate good bowel habit as in avoiding constipation, straining at stools or sitting on the toilet for long period of time. |
| |
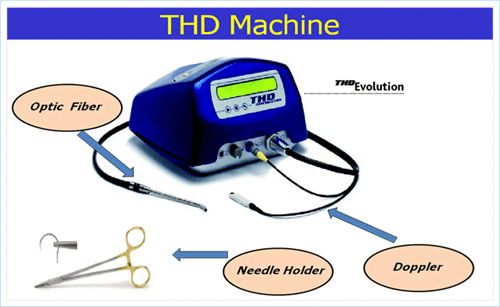
| Transanal Haemorrhoidal Dearterialisation (THD) |
| |
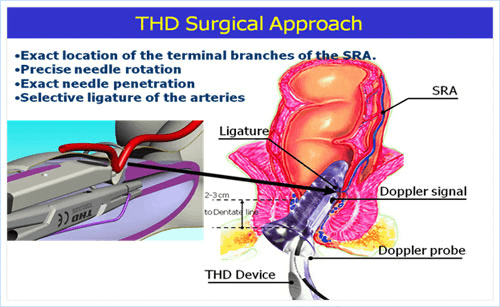
THD is the newest operative procedure for haemorrhoids to be introduced to Singapore. It utilises a specifically designed set of instruments based on the Doppler machine, to detect and stitch the feeding blood vessels of the haemorrhoids in the lower rectum.
The concept was first pioneered by Dr Morinaga, a Japanese doctor in 1995, but it has been recently modified and popularised by a group of Italian surgeons. |
| |
| The Procedure |
| |
| THD is performed under general anaesthesia or intravenous sedation and it is a day- surgical procedure. |
| |
 |
| |
| Indications |
| |
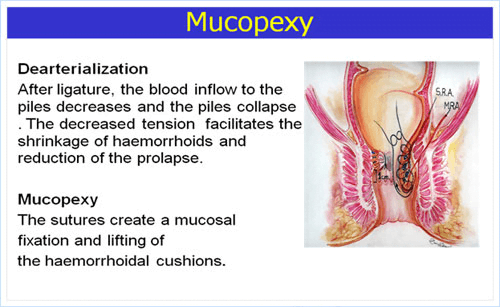
THD is effective for bleeding piles and is best indicated for recurrent Stage II piles after failed rubber-band ligations. It is extremely useful for patients who are on blood thinning medications (Warfarin, Aspirin, Plavix, or Ticlid) with troublesome bleeding piles. It is not so effective for prolapsed piles (Stage III) unless mucopexy (running stitches to lift and hitch-up prolapsed piles) is performed. |
| |
| Comparisons with Longo Stapled Haemorrhoidopexy |
| |
Like stapled haemorrhoidopexy, the operative field is in the lower rectum where there is no sensory nerve, and therefore relatively "painless". It also does not deal with skin tags which need to be trimmed separately.
Unlike stapled haemorrhoidopexy, it does not cut and remove any rectal tissue, it is therefore less invasive and should have less risk of severe complications. But without cutting and stapling, it is not as effective in lifting and hitching prolapsed piles even with mucopexy. |
| |
| Post-Operative Complications of THD |
| |
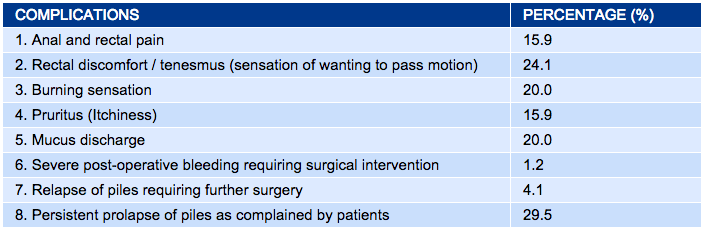
A recent publication on 170 patients from Italy shows that THD with mucopexy is effective for treating piles, but the following complications were reported: |
| |
 |
| |
| Principles And Ethics of Treatment of Haemorrhoids |
| |
Treatment of haemorrhoids depends on correct diagnosis and accurate assessment of severity. The guiding principle is to choose the right treatment for the right patient; to select the least invasive but just as effective treatment to avoid unnecessary complications; and to refrain from offering expensive operations because they are new when a cheaper treatment is just as good to prevent escalation of healthcare costs.
In the management of patients with haemorrhoids, it is as important to educate them on cultivating good bowel habit in avoiding constipation, straining at stools or sitting on the toilet for prolonged period. |
| |
| Go To Top |
| |
